The Human Milk Foundation is proud that the Hearts Milk Bank helps families facing breastfeeding challenges by providing skilled support and access to screened donor milk donated by wonderful mums. Since September 2017, the HMB has supported over 400 families outside of our hospital provision who have been referred by healthcare professionals or self referred. As our charity has grown, we wanted to ensure that this novel service was underpinned by a process that ensured safety and fairness of access to this precious resource.
In May 2019, we established a panel of volunteer experts who met at the Human Milk Foundation’s headquarters to achieve a consensus on the prioritisation of access to donor milk. The panel is formed of neonatologists, paediatricians, parents (donors and recipients), lactation specialists, milk bank team members and psychiatrist/psychologists. Initially, the panel met every 6 months, and now meets yearly to review the operation of the charity over the year and adjust guidelines going forward.
After discussion, donor milk was prioritised according to four parameters: infant vulnerability (hence NICU milk is always prioritised), maternal breastfeeding and psychological health, and milk bank supply/logistics. Sometimes, these overlap, but they give the team a broad context to manage a finite resource, and the expectations of what is possible.
In terms of duration of donor milk supply, the Prioritisation Panel set the following guidance:
For families where breastfeeding is impossible, we aim to provide 4 weeks of donor milk to allow babies to receive human milk only during the neonatal period, followed by a transitional period where formula is introduced slowly over 2-3 weeks.
- For mothers where a supply issue is being supported, there is no definitive cut off. The aim is to provide donor milk during the window of opportunity that there is to maximise maternal milk supply. The donor milk provision can therefore be very variable, and is treated on a case-by-case basis. Sometimes only a few containers are needed; at other times support can continue for several weeks.
- This is all dependent on the amount of milk that is available beyond what hospitals require, and this may mean that the HMB does not have sufficient supply to meet the needs of all families.
The key to these discussions was ensuring support to as many families as possible, being transparent in what is possible so that expectations can be managed from the outset, and a structure that is simple and fair for the team to follow.
A full list of the Prioritisation Panel members and their role is below:
- Professor Amy Brown, Swansea University (Chair)
- Gillian Weaver, cofounder of the HMF
- Shurron Rosales, mother of a donor milk recipient
- Jo Watt, IBCLC, Lactation Services Coordinator
- Felicity Webster, milk donor
- Dr Merran Thomson, Neonatologist
- Dr Andrew Long, Paediatrician
- Dr Livia Martucci, Perinatal Psychiatrist
- Wendy Jones, Pharmacist and founder of the Drugs in Breastmilk Service
- Shereen Fisher, Chief Executive of the Breastfeeding Network
- Dr Natalie Shenker, cofounder of the HMF
It is our charity’s goal that in the future we will be able to ensure that every baby and mother who could benefit from this service will be able to. If you would like to support us in this goal, please contact us.
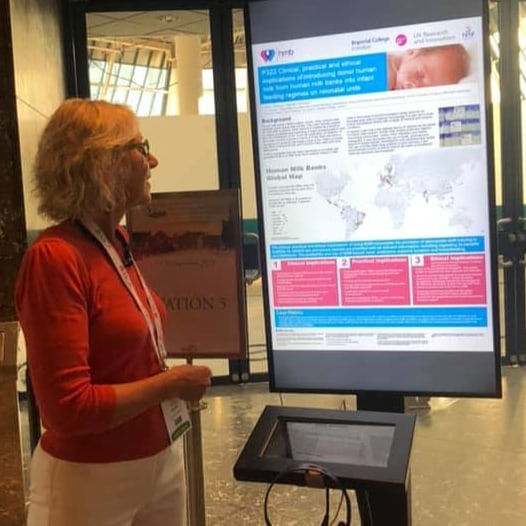
Related Publications:
Tully MR, Lockhart-Borman L, Updegrove K. Stories of success: the use of donor milk is increasing in North America. J Hum Lact 2004, 20(1):75-77.
Bramer S, Boyle R, Weaver G, Shenker N. Use of donor human milk in nonhospitalized infants: An infant growth study. Matern Child Nutr 2021:e13128.
Reimers P, Shenker N, Weaver G, Coutsoudis A. Using donor human milk to feed vulnerable term infants: a case series in KwaZulu Natal, South Africa. Int Breastfeed J. 2018;13:43. Published 2018 Sep 10. doi:10.1186/s13006-018-0185-6
Canadian Paediatric Society: Position statement. Pasteurized and unpasteurized donor human milk. 2020
Liu XH, Han SP, Wei QF, Zheng FY, Zhang T, Chen HM, Mao M. National Human Milk Bank Children Health of the Chinese Medical Doctors Association, Group of Child Health Care, Society of Pediatrics, Chinese Medical Association: The data and characteristics of the human milk banks in mainland China. World J Pediatr 2019, 15(2):190-197.
Grøvslien AH, Grønn M. Donor milk banking and breastfeeding in Norway. J Hum Lact 2009, 25(2):206-210.
Ministry of Health and Family Welfare, Government of India. National Guidelines on Lactation Management Centres in Public Health Facilities. 2017.
Wiggins PK, Arnold LDW. Clinical case history: donor milk use for severe gastroesophageal reflux in an adult. J Hum Lact. 1998 Jun;14(2):157–9.
Rough SM, Sakamoto P, Fee CH, Hollenbeck CB. Qualitative analysis of cancer patients’ experiences using donated human milk. J Hum Lact. 2009 May;25(2):211–19.
Khandelwal P, Andersen H, Romick-Rosendale L, Taggart CB, Watanabe M, Lane A, et al. A pilot study of human milk to reduce intestinal inflammation after bone marrow transplant. Breastfeed Med. 2019 Apr;14(3):193–202.