Support parents and babies
To support parents to feed their babies with human milk

The HMF was conceived in 2017 by a group of parents, scientists, milk bank experts and doctors. The initial team was fuelled by frustration at the lack of assured donor milk supply to hospitals to support the most vulnerable babies, and the countless stories of parents who wanted to access donor milk for their babies but who did not meet the criteria for donor milk use via the NHS. Families where breastfeeding was impossible could not dream of accessing donor milk except in very rare circumstances. The vicious circle of disinvestment and consequent lack of research had to be broken.
Dr Natalie Shenker and Gillian Weaver set up the UK’s first non-profit human milk bank, the Hearts Milk Bank, in 2017. While the HMB got to work sending milk into hospitals, a team came together to develop the Human Milk Foundation around Hearts. The HMF launched on the 1st August 2018, with the aim of building a new model to provide equitable access to donor human milk and breastfeeding support, and initiating vital research and education. The adventure began. In September 2024, Dr Natalie Shenker stepped down from operational responsibility for the charity to focus on her research interests with Imperial College London.

One of the leading causes of death for premature babies is a serious condition called necrotising enterocolitis (NEC). Premature infants who are exclusively formula fed or received a mixed diet are at a higher risk of developing NEC compared with infants fed exclusively human milk.

The Hearts Milk Bank has rapidly grown to provide screened donor milk to sick premature babies in over 50 NHS hospital neonatal intensive care units. The HMB also provides milk to families in the community – in our first years of operation we have sent over 10,000 litres of milk to help hundreds of families. All milk is provided free of charge under the oversight of a healthcare professional. In cases where the donor milk was used to support the mother to establish her own supply, many came back to become milk donors themselves and keep paying the kindness forward.
Alongside the provision of donor milk, the milk bank team is enabling a raft of research, including ground-breaking work into the composition of human milk over the course of natural term lactation. We collaborate with academics, scientists and milk bank experts across the UK and internationally.
To support parents to feed their babies with human milk
To supply information, education and training across the fields of human milk
To fund ground-breaking projects in human milk science
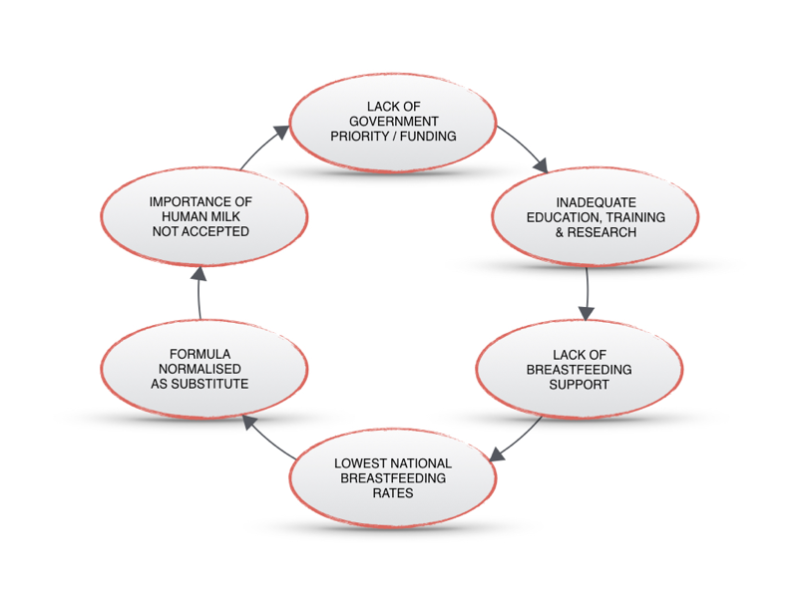
The UK has the lowest breastfeeding rates in the world with only 1% of babies breastfed at 6 months.
But the problem does not lie with mothers. More than 80% of women want to breastfeed but fewer than 50% are breastfeeding by six weeks. Breastfeeding support has collapsed with milk bank services slashed, peer support groups disbanded and lactation consultants required to self-fund training, fuelling inequality in breastfeeding success.
We need to bring together and empower voices from every culture, community and class in the UK to break this cycle of disinvestment. Feeding our babies is a universal right and a near universal challenge. The impact of non-optimal feeding is pain on an individual level and on a societal level.
Too many mothers are hurting to allow this to continue.
Together we can change this for the next generation.
HMF Co-Founders Dr. Natalie Shenker and Gillian Weaver are trusted sources of input and regularly present our work at the APPG on Infant Feeding & Inequalities. We have working relationships with members of every major political party in the UK and Ireland and are on the brink of some major developments in this area.
In 2020 Natalie and Amy Brown were invited to Number 10 Downing Street where they spoke with Prime Minister Boris Johnson about our work. We continue to make headway with Ministers in DHSC.
We have a passionate team with a diverse range of expertise in medicine, midwifery, lactation support, psychology, global communications, digital marketing, PR, event planning and business management.
We are in a unique position to be able to bring about social change as not only do we understand the medical, psychological and cultural landscape of breastfeeding but we also already have the supporting evidence for the solutions required, with published work in The BMJ, The Lancet, Journal of Maternal and Child Nutrition, Infant, RCPCH, RCM and British Association of Perinatal Medicine. Our team has a deep understanding of the history of these issues and of the importance of the WHO Code.